
The need to breathe is one of the few certainties in an otherwise uncertain world. But, did you know that how you breathe serves not only to drive energy production, but also impacts your whole mental as well as physical well-being?
Over and above providing oxygen to extract energy from the food you eat, how you breathe can have a powerful effect on heart, digestive, nerve and muscle functions as well as profoundly influencing your emotional state. Recent times have seen an increased recognition in Breathing Pattern Disorder (BPD), an abnormal breathing pattern resulting from tension, anxiety and other causes, which is responsible for a great number of common health issues
In this article, we will delve into the science of breathing and explore the concept of Breathing Pattern Disorder, uncovering its symptoms, causes, and consequences, before sharing some valuable insights into how to recognize and manage BPD to improve your health
Breathing correctly will help you reduce stress and anxiety, boost your energy, and improve your whole quality of life. Journey with us as we unlock the power of breath and take control of your breathing, your wellbeing and your life
What Is Breathing Pattern Disorder?
Breathing pattern disorder (BPD) is an abnormal breathing pattern associated with overbreathing, and linked with a number of symptoms ranging from mild to distressing. It may be mild and intermittent with few or no overt symptoms, or, at the opposite end of the scale, hyperventilation syndrome, associated with symptoms including acute breathing difficulty, heart irregularities, muscle pain and spasm, dizziness, acute fear and even fainting
Most commonly resulting from anxiety and stress, abnormal breathing can also be linked to underlying respiratory and other diseases. In a general population around 8-10% of adults are diagnosed with BPD, though the real figure is likely to be higher. This increases to around 36% in adults with asthma
The hallmark of dysfunctional breathing is excessive loss of carbon dioxide (CO2), a condition which changes blood chemistry to produce an array of symptoms including generalized muscle pain, fatigue, dizziness, irregular heart beat or pins and needles in the extremities and face. Anxiety is both a common cause, and a common symptom, providing the perfect conditions for a self sustaining vicious cycle
A normal Breathing Pattern in human adults has 3 basic features
- an average resting breathing rate of 12-18 breaths per minute
- breathing is done through the nose
- the diaphragm is the principle muscle breathing
Essential Anatomy & Function Of The Diaphragm
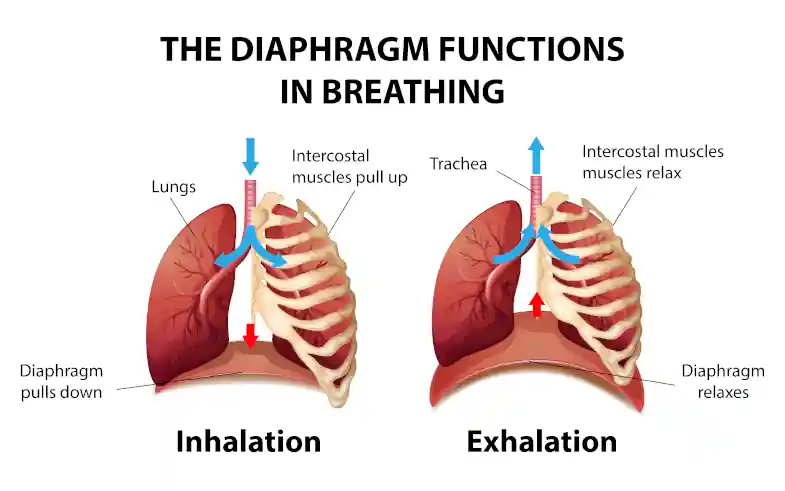
The diaphragm is a dome-haped muscle siting at the bottom of the rib cage. It is the main muscle of breathing, attaching to the lower ribs and also serves to separate the chest from the abdominal cavity During inhalation contraction of the diaphragm draws down its central tendon at the top of the dome as well as pulling the lower ribs up and out, to become flatter and wider The downward movement of the chest cavity floor enlarges the cavity (thorax), decreasing it’s pressure which is filled by air entering the lungs During exhalation the diaphragm simply relaxes, the rest being achieved by the elastic recoil of the rib cage, intercostal muscles and lungs. At the end of exhalation the lungs remain filled with a quantity of air, forced exhalation being beyond this being achieved primarily by the abdominal musclesDiaphragmatic v Upper Chest Breathing
Diaphragmatic breathing draws air deep into the lower lungs where their volume is greatest to maximize gas exchange. It is an efficient way to breathe yielding the maximum effect with the least effort Rib breathing happens through the action of the intercostal muscles between the ribs and accessory muscles of the neck (Scalenes). While lower rib breathing assists the action of the diaphragm, upper chest breathing requires a much greater muscular effort. Unaided by the diaphragm the shallower breathing pattern also needs to be faster to compensate Upper chest breathing is associated with greater muscular tension in the upper chest and back as well as the shoulder, scapular and neck muscles. There is also a strong link with head forward posture which, once established, maintains the neck and shoulder muscles tension to produce dull aching pain and fatigue. Tension type headache is a not uncommon consequence of such a postural pattern and is a common symptom of BPD While upper chest breathing is not in itself indicative of overbreathing, its fast and shallow pattern and association with neck and shoulder pain make it a good candidate for setting up dysfunctional breathing. Where BPD is confirmed breath retraining to favour the diaphragm is an imperativeMouth v. Nose Breathing
Mouth breathing may occur as a result of blocked nasal passages, or as a chronic habit, often from childhood. In addition to moistening and filtering inhaled air, nose breathing serves a number of other functions: Nose breathing offers a degree of resistance to air flow which helps inflate the lungs to improve breathing efficiency. This is well illustrated in people with Chronic Obstructive Pulmonary Disease (COPD) who spontaneously adopt a pursed-lip breathing strategy to help keep the airways open The passage of air through the nose also stimulates the mucous membranes to release nitric oxide, or NO (not to be confused with the “laughing gas” nitrous oxide), which is inhaled into the lungs. The effects of NO on the respiratory system include- vasodilation – widening of the blood vessels to improve oxygen and carbon dioxide exchange and transport
- bronchodilation – opening of the airways for improved air flow
- immune function – NO is anti bacterial, anti-fungal and anti-viral
Overbreathing produces its effects through the excessive loss of carbon dioxide (CO2) during exhalation. Acidic when dissolved in water (blood), loss of CO2 shifts the blood pH (acid-alkali scale) towards the alkaline, triggering a number of responses in multiple body systems
Below is a short account of the mechanisms and physiological changes associated with the symptomatology of respiratory alkalosis
If you prefer, you can skip the section and jump straight to the list of symptoms associated with BPD
For a broad introduction to the respiratory system check out this 10 minute educational video by Osmosis
Physiology Of Breathing And Overbreathing: a 3 Minute Crash Course
- Breathing supplies oxygen (O2) for energy, while expeling carbon-dioxide (CO2), a waste product of energy production
- Where oxygen is relatively pH (acid-alkali) neutral, CO2 is acidic
- Your brain has evolved to detect CO2 levels by reading the blood pH: acid = more CO2, alkali = less CO2
- Detecting excess CO2 the brain quickens the breathing and heart rate to expel more of it and return the blood gases to balance
- Exertion produces more CO2, which stimulates the breathing to expel CO2 and make the blood less acidic (more alkaline), in turn slowing down the breath back to resting rate – at least that’s what should happen
Stress, anxiety, and factors including pulmonary disease, postural imbalances and structural issues affecting the neck, upper back, rib cage and diaphragm can all lead to fast shallow breathing, ovewrrideing the body’s corrective mechanisms. Loss of CO2 sends the blood pH too far towards the alkaline range of the scale (respiratory alkalosis)
Respiratory alkalosis is associated with feelings of anxiety and stress, stimulating the fight-and flight response via the sympathetic nervous system, establishing a perfect viscious cycle
While decreasing CO2, overbreathing also increases O2 levels: unfortunately alkalosis keeps O2 bound to your red blood cells, rather than being released into the tissues, these becoming oxygen deprived. Alkalosis also reduces the availability of calcium, essential for muscle and nerve function, by in turn keeping it bound to blood proteins (albumin)
The reduced availability of O2 and Calcium from respiratory alkalosis disturbs muscle and nerve function, with symptoms such as muscle cramps, tingling and dizziness. Smooth-muscle contraction leads to narrowing of the blood vessels and digestive tract, restricting blood flow and disturbing gastro-intestinal function
The Impact Of Altered Breathing Pattern
on your physical and mental health
Symptoms Of Dysfunctional Breathing
As many as 30 breathing pattern disorder symptoms have been identified. Some of the more common ones include:
- Frequent sighing & Yawning
- Air hunger: a sense of not being able to have a satisfying breath in
- tingling and pins-and-needles in the extremities and face, especially around the mouth, and on occasion even in the tongue
- abdominal cramping and a general sense of indigestion
- racing or irregular heart beat
- sleep disturbance: difficulty falling asleep; waking often
- sweating, especially in the hands
- dizziness and light headedness
- brain-fog, mental confusion, inability to focus
- anxiety and hypervigilance
- possible panic attacks if severe
- general fatigue
- Sore, aching muscles
How you breathe can significantly impact on your physical and mental health. Physically, dysfunctional breathing leads to poor oxygenation of tissues and organs, resulting in fatigue and muscle tension. There is also an association with chronic pain syndromes, though comes first is debatable.
For example, dysfunctional breathing patterns are common in people with fibromyalgia, a chronic condition of unknown origin which produces widespread pain, fatigue and other symptoms. Though it’s likely the breathing disturbance is secondary to being in pain, breath retraining has been shown to help with fibromyalgia associated pain (Núñez et al 2024)
The interplay between breathing and mental health is complex and profound; the disorder can exacerbate feelings of anxiety, depression, and stress, which in turn leads to altered breathing establishing a vicious cycle
In the social realm, individuals with BPD may avoid social situations and activities for fear of experiencing symptoms in public, resulting in isolation and reduced social interaction. Such avoidance behavior can exacerbate feelings of loneliness and depression, further impacting mental health
All of this serves to highlight the importance of dealing with BPD holistically, addressing not just the physical, but also the psycho-social correlates. In addition to breath retraining, effective management will need to explore the individual’s emotional responses, providing a supportive environment where individuals can safely explore and express their challenges and seek help without stigma
Diagnosing Dysfunctional Breathing Patterns
The symptoms of BPD can mimic other medical conditions, making diagnosis challenging. Symptoms such as rapid breathing, for instance, can be mistaken for asthma or other respiratory disorders, while the psychological aspects can resemble generalized anxiety disorder. This overlap highlights the importance of a comprehensive evaluation by a healthcare professional to accurately diagnose BPD and implement appropriate interventions
The first step in the diagnosis of breathing pattern disorder begins with a thorough understanding of the individual’s medical history and symptoms. This initial conversation is essential in determining whether dysfunctional breathing may be at play, and identifying some of t he major triggers and causes
Patients often report a variety of experiences that can seem unrelated, such as persistent fatigue, feelings of anxiety, or chest discomfort. By asking you to describe your symptoms in detail, including when they began, their frequency, and potential triggers the healthcare practitioner can identify patterns that suggest BPD and / or the need for further investigations
Following the history, the practitioner will usually also perform a physical examination. This may include listening to the heart and lung sounds and assessing respiratory rate, etc.
More specific diagnostic tools such as pulse oximetry, to measure the oxygen saturation in the blood, and spirometry and peak expiratory outfow rate (PEOR) may be used to more fully evaluate lung function
The objective is to rule out underlying respiratory conditions before confirming the symptoms correspond to breathing pattern disorder
Having established BPD as the cause, more comprehensive evaluations may involve assessing the breathing pattern during various activities, especially under stress or during exercise. Specialized breathing assessments, such as the Buteyko and Papworth method which involve observing the patient’s breathing while they engage in deep relaxation or controlled breathing exercises. These evaluations can help to pinpoint specific dysfunctional breathing habits and point to appropriate corrective intervention
The diagnostic process may include psychological assessment, as there is often a significant interplay between anxiety and dysfunctional breathing. Mental health professionals can explore whether anxiety, panic attacks, or other psychological factors are exacerbating the breathing issues.
Also important is to distinguish between acute and chronic forms of breathing pattern disorder. Acute conditions may arise from specific incidents, such as a panic attack or an asthma exacerbation, while chronic conditions stem from long-standing habits or emotional tension
Where an underlying pathology has been identified, a multidisciplinary approach is desirable. Collaboration between cardiologists, respiratory medicne specialists, psychologists, and other healthcare professionals ensures that all potential co-factors are explored for a comprehensive diagnosis of the patient’s condition.
This holistic approach allows healthcare providers to collaborate with the patient in developing a actionable management plan. This may include breathing retraining exercises, lifestyle modifications, and psychological support. The goal is to equip you with the tools necessary to regain control over your breathing and improve your overall quality of life
Managing Your Breathing Pattern
Through Breath Awareness And Mindfulness Techniques:
One of the most effective ways to manage breathing pattern disorder is through applying breath awareness and other mindfulness techniques. By cultivating an awareness of one’s breathing, individuals can begin to recognize patterns and triggers that contribute to their BPD
Simple practices such as mindful breathing involve focusing on each inhalation and exhalation, allowing you to become more attuned to your body and the sensations associated with breathing. Better breath awareness can help break the cycle of maladaptive breathing, providing you with a valuable tool to regain control of your breath
Other mindfulness techniques can also play a crucial role in reducing anxiety and stress, two common contributors to BPD. Engaging in mindfulness meditation or guided breathing exercises encourages relaxation and promotes a sense of calm. These practices focus on grounding you in the present moment, allowing you to acknowledge and accept your feelings without judgment. Beyond a formal practice session, integrating mindfulness into your daily routines will help notice the relationship between your breath and your emotions, helping to break the cycle and developing a greater sense of freedom and peace
Incorporating breath awareness into physical activities can further enhance the management of BPD. Practices such as yoga, tai chi, or even simple stretching will help connect movement with breath to promote an immediate sense of physical wellness. These activities also encourage deep, diaphragmatic breathing over chest-based breathing to calm the breath, reduce tension and cultivate overall well-being
Getting Professional Help
While self-management techniques can be beneficial, seeking professional help may be the better option for individuals struggling to manage breathing dysfunction. Health professionals, such as respiratory therapists, psychologists, or specialized counselors can offer tailored interventions to address both the physical and psychological components of BPD. A thorough assessment by a healthcare provider can help identify the deeper issues contributing to the disorder, allowing for a more comprehensive management plan
Cognitive Behavioral Therapy (CBT) has shown promise in treating BPD. CBT focuses on identifying and modifying negative thought patterns that contribute to anxiety and stress. By addressing the cognitive aspects of disordered breathing, individuals can learn coping mechanisms and techniques to manage their symptoms more effectively. The therapy can also include exposure techniques to gradually confront situations that trigger anxiety, thereby reducing the fear associated with altered breathing patterns
Specialized breathing retraining programs led by trained professionals can also provide the skills necessary to develop healthier breathing habits. These programs often include exercises that focus on diaphragmatic breathing, breath control, and relaxation techniques. Working with a therapist can also help with compliance, encouraging participants to stay committed to their journey toward a healthier life
Life-Style Changes For Preventing And Managing
Stress Related Breathing
Preventing and managing stress-related breathing patterns require a proactive approach that encompasses simple lifestyle changes, stress management techniques and regular self-care. One of the most effective strategies is to incorporate stress reduction practices into daily life. Activities such as regular exercise, meditation, and engaging in hobbies can significantly lower stress levels, reducing the likelihood of developing or exacerbating BPD. Finding time for relaxation and self-care is essential for maintaining a balanced mental and emotional state
Adequate sleep, a healthy nutritious diet, and proper hydration are vital components of overall well-being. Poor lifestyle choices can lead to increased stress and disordered breathing. Simple changes, such as practicing good posture, going for a walk and taking regular breaks between periods of sitting can also help avoid tension and enhance breathing efficiency
Finally, fostering a supportive environment is crucial for managing stress-related BPD. Surrounding yourself with understanding friends and family and communicating openly about one’s struggles can help alleviate feelings of isolation and encourage others to offer support. A supportive network is a valuable resource for stress management, helping you take significant steps toward preventing and managing BPD
Conclusion: Embracing a healthy breathing pattern
The journey toward better breathing is not just about addressing a disorder; it is about cultivating a deeper connection with ourselves. The way you breathe profoundly affects your physical and mental state, impacting our overall quality of life. Understanding the multiple facets of healthy and dysfunctional breathing is essential for achieving optimal health and well-being. By recognizing the symptoms and causes of BPD, you can take proactive action to break free from the cycle of maladaptive breathing and embrace new habits to live a fuller and happier life
The Mind Body Connection: Finding Health In An Age Of Stress
What Is The Mind Body Connection?Since the intention of this blog is to explore the many facets, practices and benefits of natural health and healing, it seems apt to begin our journey with a discussion of a central pillar of natural healing: the mind body connection...
Yoga And Mindfulness For Dysfunctional Breathing: 5 Exercises For Better Health
Did you know breathing too much carries a health warning? Beyond gas exchange, how you breathe affects all your systems, from digestive and cardiovascular function to emotional health
Rest And De-stress: The Vagus Nerve And Yoga
Overwhelmed, stressed, or in need of a quiet moment? Just find a quiet place, sit or lie down, and find inner your tranquility through the healing power of the Vagus nerve
